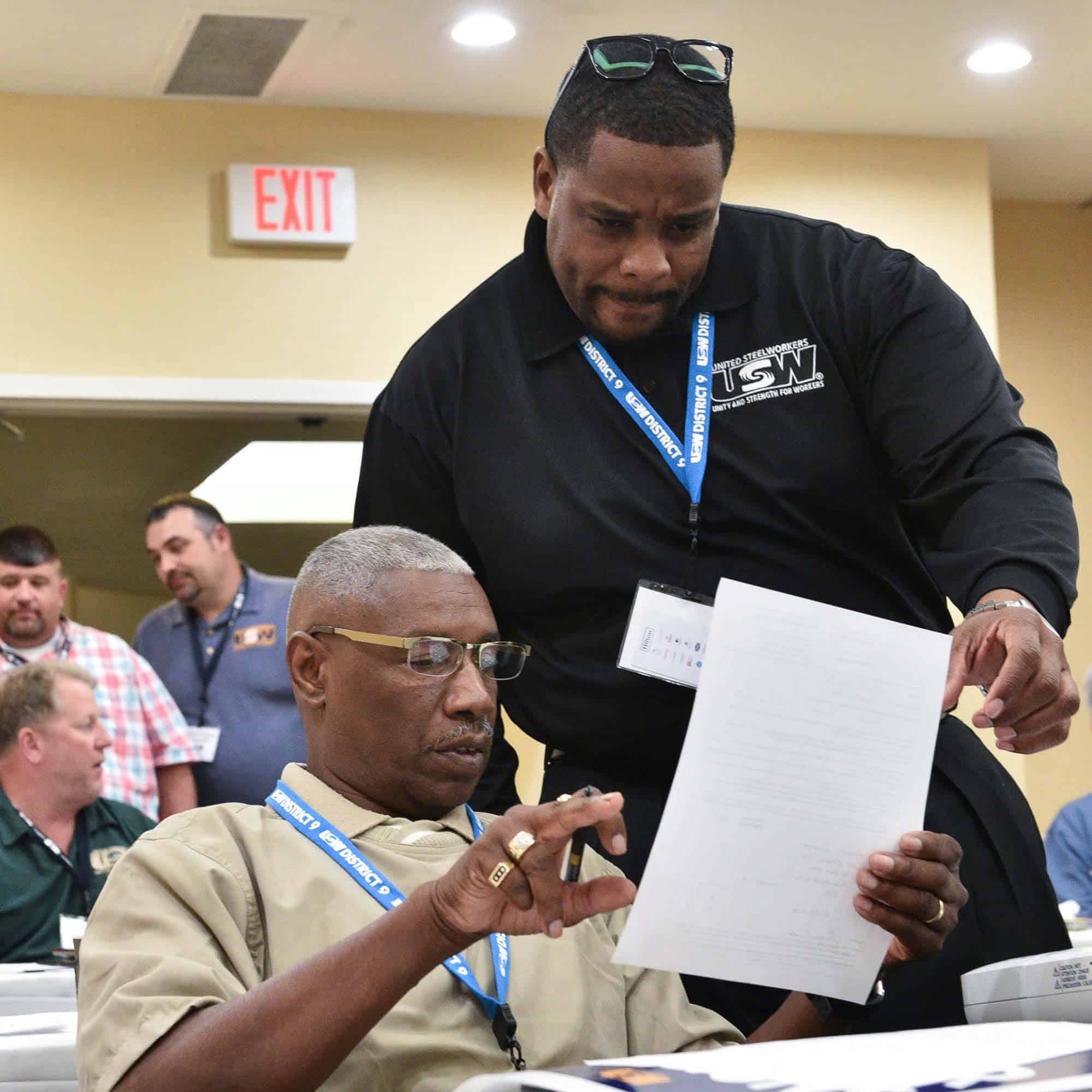
For Members
This is our union and together, we’re fighting shoulder to shoulder for each other, our families, and our futures. Below find links to resources and information to help aid in this work or contact us with any questions.




Need Something Else?
Let Us Know!
The USW is here to help our members find resources and information and answer any questions you may have.